While there is a growing number of cancer-focused startups, the reality is that cancer is one of the most common diseases with a high fatality. While immunotherapies have transformed treatment for some blood cancers, they’ve had limited success against solid tumours.
One UK biotech thinks the answer lies not in ever more targeted drugs, but in the body’s oldest line of defence: neutrophils. LIfT BioSciences is a UK biotech company working on a new kind of cancer treatment.
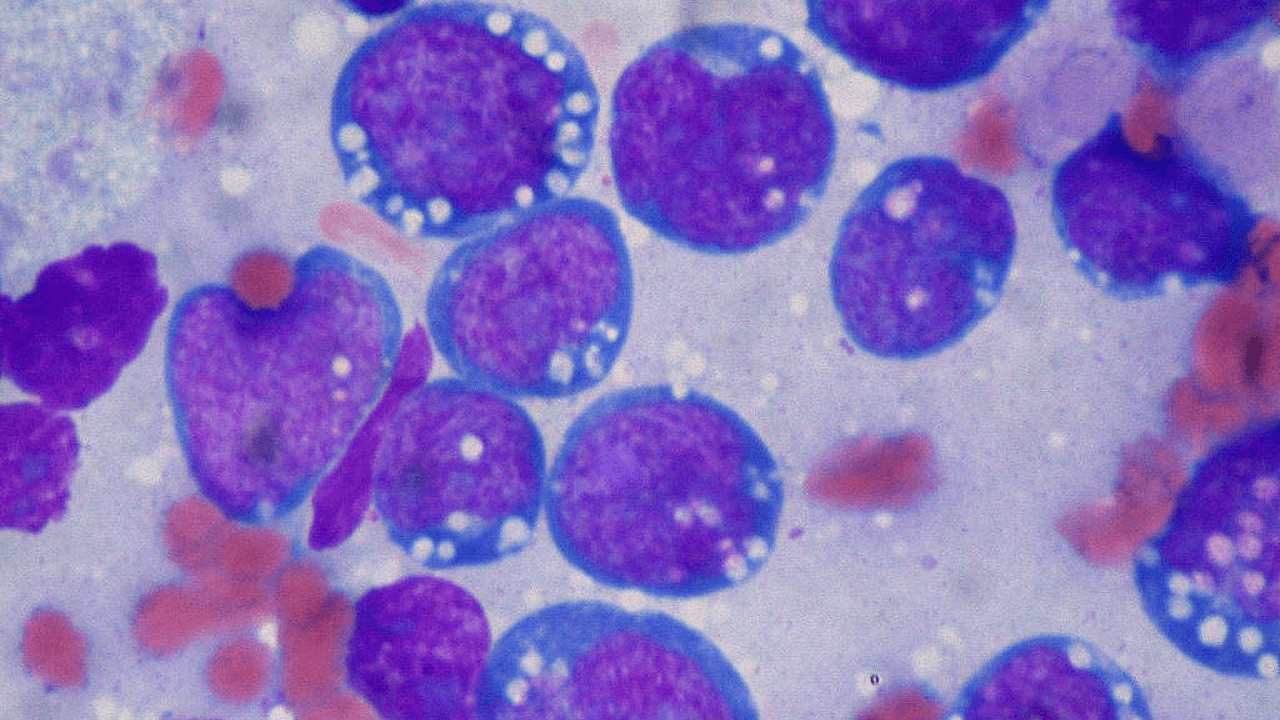
Instead of using T-cells (like many current immunotherapies), they focus on neutrophils — a type of white blood cell that we are all born with that’s part of the body’s first line of defence.
LIfT engineers these neutrophils so they can better find and kill cancer cells, and also help the rest of the immune system join the fight.
The company is still in the early stages of development, but has secured patents, research partnerships, and funding to move the technology forward. Its goal is to create a scalable cell therapy that works against solid tumours — types of cancer that are often hard to treat with existing methods.
I spoke to CEO Alex Blyth to learn more.
“Find My Nearest” to finding a cure
Blyth is a serial entrepreneur and inventor with a background in biology and economics. He began his career in the dot-com industry. He recalled:
“When I was at university, I built and sold a company that created the world’s first 'find my nearest' technology for mobile phones.
It took just two years from start to sale.”
Since then, he’s worked with major pharma companies to bring novel biopharma assets to market. However, when his mother was diagnosed with pancreatic cancer, he witnessed firsthand how targeted therapies ultimately fail:
“Watching my mother die on Abraxane, a drug I had worked on, made me realise that this targeted drug approach is fundamentally flawed for a moving target like cancer.”
He detailed:
“Tumour cells adapt under evolutionary pressure, escape the drug, and patients die from tumour escape — metastases that evade the immune system.
In fact, 90 per cent of cancer deaths result from metastases, not primary tumours. And yet, the vast majority of oncology research focuses on identifying new targets. Most meetings start with: “What’s our target?” But that’s the wrong starting point.
Approximately 90 per cent of industry resources are allocated to targeted or fixed-modality therapies. These approaches can debulk tumours and extend life slightly, but they don’t prevent antigen escape, which ultimately kills the patient.”
As a result, he began examining individuals who don’t develop cancer, and discovered that their immune systems possess a remarkable ability to distinguish between friend and foe.
He recalled: “I conducted donor studies comparing immune cell types in “super donors” with no history of cancer versus those who had it.
The standout cell was the neutrophil.
Neutrophils are a type of white blood cell that play a crucial role in your immune system by helping to fight infections and heal injuries. They are the most abundant type of white blood cell, making up approximately 50 to 70 per cent of all white blood cells in the body.
How neutrophils slipped through the cracks of cancer research
According to Blyth, the neutrophil is “the most corrupted cell in cancer patients compared to super donors, and it’s also the most abundant white blood cell in the body, making up 70 to 80 per cent of cells in a tumour. Yet neutrophils have been almost completely overlooked in cancer research.”
He attributes this to four main reasons:
First, they’re challenging to handle. Neutrophils are like the “puffer fish” of the immune system. When you take them out of the body, they’re incredibly fragile and survive only 12 to 24 hours, unlike hardy T-cells.
Second, they don’t fit the industry’s binary model. T-cells work through inhibitors and agonists, which fits with how pharmaceutical companies — fundamentally chemistry companies — understand science. Neutrophils use advanced, non-binary threat pattern recognition, and many scientists are uncomfortable with mechanisms they can’t fully explain.
Third, he contends that people used to think the innate immune system only fought bacteria and external threats:
“In fact, it plays a key role in spotting and destroying anything that doesn’t belong — including worn-out cells and cancer cells. It’s also responsible for fine-tuning “friend vs foe” recognition inside the body.
This system can weaken over time due to ageing, stress, and changes in gene expression. Some people are born with naturally stronger innate immunity, which may explain why certain families have little or no history of cancer.”
Fourth, Blyth contends that pharmaceutical companies make money using low-risk technologies — such as antibodies and small molecules — so there’s little incentive to take career risks on new approaches.
“It’s not that companies are 'evil'; it’s human nature. Most people in science are cautious rather than trailblazers. They build safe careers inside big pharma or VC firms, and that passive self-interest kills innovation.”
Turning “super donors” into cancer fighters
LIfT’s approach involves injecting healthy neutrophils into patients, but with a twist: these neutrophils are grown in the lab from stem cells donated by “super donors.”
Super donors are individuals whose immune cells display exceptional cancer-killing abilities. By using their stem cells, LIfT can generate large batches of potent neutrophils in the lab.
These cells — a unique type of innate immune cell called Immunomodulatory Alpha Neutrophils (IMANs) — behave entirely differently from the defective neutrophils typically found in cancer patients.
Once produced, they are infused into the patient’s bloodstream via IV, providing a powerful, temporary boost to the body’s innate immune system to help combat cancer.
“The hardest thing I’ve ever done”
Biotech is, by necessity, a slow and cautious field. I wondered how Blyth reconciled this with the speed of the startup world. He admits that it has taken him ten years for the company to get to its current stage:
“It’s the hardest thing I’ve ever done, even with two previous exits under my belt.
Biotech is slow and cautious for good reason — almost everything you put in someone’s body has the potential to do more harm than good.
What pains me is knowing that nearly a million patients die every month from untreated tumours.
I’ve lost friends along the way. It’s heartbreaking to watch people die knowing that we might be able to help but can’t intervene without jeopardising the entire clinical program — or risking my own position.”
Then there’s the incremental nature of fundraising.
Blyth asserts that “If someone had given me the total amount we’ve raised so far, up front, I could have done this in half the time.”
Another obstacle is a lack of belief that cancer can be cured. Blyth explained that “pharma companies aren’t even allowed to use the word “cure,” which affects how people think.”
“But we’ve already seen immunotherapies cure blood cancers. Checkpoint inhibitors have given some patients with solid tumours a real shot at being cured. It is possible — the mindset just hasn’t caught up yet.”
The crucial 1 per cent who push boundaries
Blyth admits that he’s learnt that “you only need the 1 per cent — the people who really get it and care enough to do something."
"These people tend to find each other. Over time, I’ve met many of the pioneers who worked on checkpoint inhibitors, for example, through different paths. There’s a small, tight-knit community of people who keep pushing, often outside the establishment. The public doesn’t realise how small this group is. Most funding still goes to universities and trend-driven research, where the incentives are to publish, not to solve real-world problems. Unless you have a personal mission, the system pushes you towards career progression, not breakthroughs. I focus on finding and working with that exceptional few," he shared.
LIfT BioSciences has raised over $38.4 million, including an €11.9 million Enterprise Ireland grant for a clinical trial in Galway. This investigator-initiated trial will focus on cervical, head, and neck cancers, with first patient dosing scheduled for next year.
Lead image: Wikipedia.


Would you like to write the first comment?
Login to post comments